Services
Conditions that we treat
Our specialist is well established internationally, having been invited to give lectures in many parts of the world and appointed to several working groups responsible for developing international clinical practice guidelines. With a strong scientific and clinical background, we provide evidence-based treatment based on the results of latest clinical trials, focusing on the patient’s quality of life and clinical outcomes.”
Do note:
- The clinic is licensed to provide remote consultation services.
- Any person who needs any essential life saving measure should not seek to receive such measure by remote provision from the licensee.
Smooth & Supportive Patient Journey
Emphasis on Education & Prevention
Coordinated & Evidence- Based Treatments
Specialist Consult
Arrange to meet our kidney specialist face-to-face, so that they can take a detailed history and perform a physical examination, and assess the clinical symptoms or abnormal investigation results you may have. Our specialist will address all your concerns and provide you will a clear and detailed explanation about your condition, and propose a diagnostic evaluation and treatment plan, based on the latest clinical evidence and information, as an overall solution to your health issues.
Kidney Symptoms
Unfortunately, most kidney diseases do not present with symptoms until there is leakage of massive amount of protein in the urine or when the kidney function is significantly damaged. Most often, kidney diseases are uncovered when abnormal blood or urine test results are obtained during health screening.

- Blood and/or protein in the urine
- Elevated serum creatinine levels, or reduced kidney function
- Cysts detected on kidney ultrasound
- Passing visible blood in the urine (hematuria)
- Frothy urine
- Pain on urination
- Leg swelling
- Eyelid swelling
- Breathlessness
- Nausea and vomiting
- Left sided and/or right sided back pain
- Loss of appetite and/or weight loss
Kidney Conditions
The following provide you with some basic information on common kidney conditions. They are not meant to substitute a consult with your kidney specialist, but to provide some background understanding of the respective kidney disease.
Select Service
Specialist Consult
Arrange to meet our kidney specialist face-to-face, so that they can take a detailed history and perform a physical examination, and assess the clinical symptoms or abnormal investigation results you may have. Our specialist will address all your concerns and provide you will a clear and detailed explanation about your condition, and propose a diagnostic evaluation and treatment plan, based on the latest clinical evidence and information, as an overall solution to your health issues.
Kidney Symptoms
Unfortunately, most kidney diseases do not present with symptoms until there is leakage of massive amount of protein in the urine or when the kidney function is significantly damaged. Most often, kidney diseases are uncovered when abnormal blood or urine test results are obtained during health screening.

- Blood and/or protein in the urine
- Elevated serum creatinine levels, or reduced kidney function
- Cysts detected on kidney ultrasound
- Passing visible blood in the urine (hematuria)
- Frothy urine
- Pain on urination
- Leg swelling
- Eyelid swelling
- Breathlessness
- Nausea and vomiting
- Left sided and/or right sided back pain
- Loss of appetite and/or weight loss
Kidney Conditions
The following provide you with some basic information on common kidney conditions. They are not meant to substitute a consult with your kidney specialist, but to provide some background understanding of the respective kidney disease.
Kidney Biopsy
What is a Kidney Biopsy?
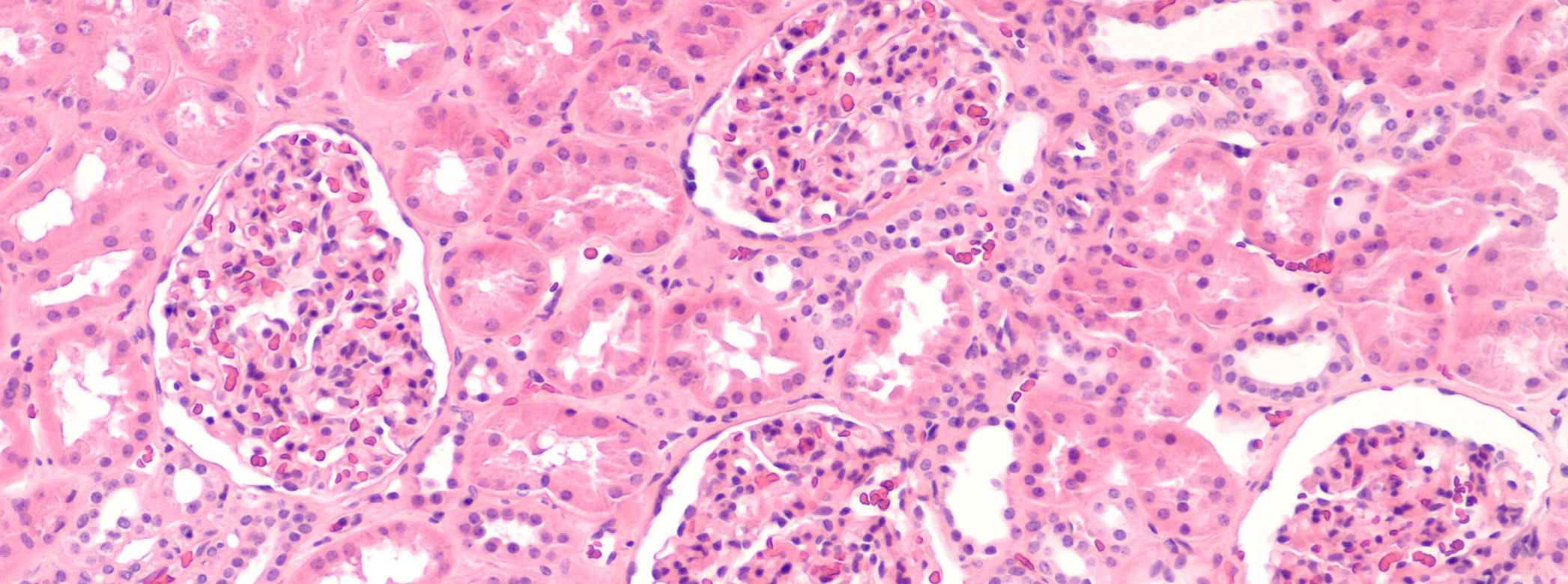
- A kidney biopsy involves obtaining 2-3 very small samples, each about 1 cm in length, from one of your kidneys using a special needle.
- The samples can then be processed and tested under the microscope to find out the cause of your kidney disease, how active the disease is or how much scarring there are in the kidneys.

Why do I need this procedure?
- Although many kidney problems can be diagnosed from your symptoms, physical examination, blood tests and scans, there are others for which direct examination of your kidney tissue is essential to make a precise diagnosis and plan treatment.
- Examples include unexplained protein or blood in the urine, swelling in your legs or other parts of the body due to excessive protein leakage in the kidneys, un explained poor kidney function or kidney failure or an assessment of kidney damage in conditions such as systemic lupus erythematosus (SLE).
- The pathologist reading your biopsy samples will be able to tell if there is inflammation of the filters in the kidneys, which is called glomerulonephritis, or other forms of damage that can account for the kidney problem.
- Your kidney specialist will only request a kidney biopsy if it is necessary to help make the correct diagnosis and plan your treatment. He or she will tell you what is being looked for and answer any questions you may have about the procedure.
What are the preparations before the biopsy?
- A simple blood test to check your clotting ability will be done before the procedure.
- If you are taking any blood thinning medication such as Aspirin, Ticlodipine or Clodiprogel, you will have to stop the medication at least 5 days before the procedure.
- There is no other preparation required on your part, and there is no need for you to omit food or drinks before the procedure.
- Please also continue to take your other medications, unless instructed by your kidney specialist.
How is the procedure performed?
- The biopsy is performed under ultrasound scan guidance.
- You will lie on your stomach and the ultrasound scan will be used to identify a point over one kidney for the biopsy.
- A small needed will be used to inject local anaesthetic into the skin, fat and muscle area above the kidneys, so that it will become numb and you will not feel any pain thereafter.
- Once the area is numb, the biopsy needle will be passed to your kidney and a small piece of kidney tissue will be obtained with the press of a button.
- Two to three pieces are usually needed, so as to obtain enough tissue for diagnosis.
- You will feel a pushing sensation but it should not be painful, and only one kidney is biopsied.
- A dressing will be applied and you will be asked to remain lying flat in bed, to allow your body to compress on the biopsy area, for about 8 hours.
What are the risks and complications of the procedure?
- In about 1 in 10 biopsies, there is visible bleeding in the urine that will usually settle spontaneously.
- In less than 1 in 50 biopsies, there is more bleeding that requires a blood transfusion.
- In less than 1 in 1,500 biopsies, the bleeding may continue and require urgent X-ray scans or even an operation to stop the bleeding.
- In less than 1 in 3,000 biopsies, the kidney may have to be removed to stop the bleeding.
What do I expect after the procedure?
- After the biopsy, you will be asked to rest in bed for at least 8 hours.
- Your pulse rate and blood pressure will be monitored and when you pass urine, it will be tested for bleeding.
- During this time, you can eat normally and will usually be encouraged to drink plenty of fluids, unless instructed by your kidney specialist not to do so.
- When the local anaesthetic wears off, you may feel some soreness over the back, for which you can be given a mild painkiller.
- A provisional result of the biopsy should be available within 48 hours, but the full report may take longer.
- If you feel well after the biopsy and have no pain or bleeding, you may be able to go home later the following day to rest.
- After the biopsy, you should avoid exercise and not carry heavy weights for 2 weeks.
- If you develop severe pain around the kidney or notice any blood in your urine, you should contact your kidney specialist straight away.
Is there any other option?
- A kidney biopsy is usually the last test to be done to investigate the cause of your kidney problem, because the other tests have not provided any better answer.
- Without a biopsy, your doctor may not be able to advise the best treatment for you, and the kidney damage may progress and become irreversible.
What will happen if I do not undergo the procedure?
- Your kidney specialist will tell you what changes in treatment could be made for your kidneys if you decide not to have a kidney biopsy taken first.
- He or she will also inform you of the risks of kidney damage and the potential outcomes.
Chronic Kidney Disease Management
Our specialist is a renowned expert in the management of diabetic kidney disease, the most common cause of kidney failure in Singapore, and have experience in successfully implementing chronic kidney disease management program. We have a structured program in screening for chronic kidney disease and implementing interventions to slow down the progression of kidney damage. You will be informed of the treatment goals, management plans and progress of your condition, with your care coordinated across other specialists and healthcare professionals where necessary.
What is Chronic Kidney Disease?
- Chronic kidney disease is the term used to describe a gradual loss of kidney function due to diseases affecting the kidneys.
- Often the damage to the kidneys is irreversible and as long as the diseases are present, the loss of kidney function will progress until advanced kidney failure occurs, where dialysis or kidney transplantation would be necessary to sustain life.
- The most common cause of chronic kidney disease in Singapore is diabetes mellitus and high blood pressure.
- Other causes include inflammation of the kidneys called glomerulonephritis, kidney stones, prolonged use of painkiller drugs or genetic diseases such as polycystic kidney diseases.
Screening for Chronic Kidney Disease
- People with conditions at high risks of kidney damage, such as diabetes or high blood pressure, should be screened for chronic kidney disease.
- Screening is usually done through blood and urine tests, looking for elevated toxins in the blood, and protein and/or blood in the urine.
- People with diabetes or high blood pressure should undergo screening at least annually, as interventions during the early stages of chronic kidney disease may slow down the progression or even prevent kidney failure.
- Screening for chronic kidney disease with similar blood and urine tests may be performed for the general population, though the cost-effectiveness of this had not been determined.

Slowing the Progression of Chronic Kidney Disease
- Your kidney specialist will control the risk factors that are associated with the progression of chronic kidney disease, including high blood pressure and uncontrolled blood sugar levels.
- Lifestyles modifications such as reducing the salt intake, smoking cessation, exercise and weight reduction have also been found to be effective in slowing the kidney damage. Your kidney specialist will review with you, the necessary treatment plan, so that these can be achieved in an effective and sustainable manner.
- Your kidney specialist may also start you on medications that have been shown to protect the kidneys. These drugs may be specific high blood pressure or diabetes medications, and often close monitoring for their effectiveness and possible effects are necessary.
Managing Complications of Chronic Kidney Disease
- As kidney disease progresses, complications could arise that may affect your quality of life and daily activities.
- These include anaemia, poor bone quality, skin itching, excess toxin accumulation and water retention.
- Your kidney specialist will screen for these complications early, often through specific blood investigations, and adjust your medications in a timely manner to ensure your comfort.
Dialysis
Dialysis is the most immediate way of maintaining the excretory function of the kidneys, to ensure the sustenance and improve the quality of life for people with advanced kidney failure. Time is needed to prepare someone for dialysis, and studies have shown that patients who start dialysis in a prepared manner rather than on an emergency basis, have better outcomes. Do talk to your kidney specialist to decide on the most appropriate time for you to start preparing for dialysis, when is the best time to begin actual dialysis treatment and what dialysis treatment is best suited for your medical condition and lifestyle. We have a comprehensive education and counselling program for people with kidney failure and needing to start dialysis, and will coordinate your care to ensure that dialysis, when required, is started in a timely manner with minimal disruption to your lifestyle.

Hemodialysis (Blood-Based form of dialysis treatment)
What is Hemodialysis?
- Hemodialysis or HD is a blood-based form of dialysis treatment, where blood from the body goes through a machine and a special filter called a dialyser, and toxins and excess water are removed before the blood is returned back to the body.
- This is a continuous process performed over about 4 hours each session, and usually 3 sessions a week are required to maintain the health and comfort of a patient with advanced kidney failure.
What are the preparations required?
- To extract adequate blood from the body over 4 hours with sufficient blood flow rate, a large enough vein must be available.
- This vascular access is called an arteriovenous fistula or AVF. This is achieved through a small surgical procedure in one of your arms, either at your wrist area or around the elbow region.
- The surgical procedure involves connecting an artery to a vein, so that blood from the artery can flow at high volume and speed into the vein, making it bigger with thicker walls so that it becomes suitable for hemodialysis.
- The surgery is usually performed as a day surgery procedure, but it takes time of about 8 to 12 weeks for the vein to mature to an appropriate size for use.
How is Hemodialysis performed?
- In Singapore, you will have to go to a Hemodialysis Centre to receive your dialysis treatment.
- Your kidney specialist will be able to arrange an appropriate centre for you, where treatment is performed usually 3 times a week, with each session lasting about 4 hours.
- Two needles will be inserted into the length of your AVF, about 6 cm apart from each other.
- One needle will be used to extract the blood from your body to go through the dialysis machine, and clean blood from the machine will then be returned through the other needle.
- Roughly about 150-500 millilitres of blood every run through the machine every minute during the treatment.
- To prevent your blood from clotting during the 4 hours of treatment, an anti-clotting medication called Heparin, will be infused continuously through the machine unless decided otherwise by your kidney specialist.
What are the risks of Hemodialysis?
- As blood is removed continuously from your body during the treatment, and water is also extracted by the dialysis machine, your blood pressure may decrease, and you may experience some giddiness or leg cramps.
- The low blood pressure, if too severe or prolonged, may increase the risk of a heart attack.
- Since this is a blood-based therapy, there is a risk for blood-borne infections, including bacteria getting into the blood which could cause infections anywhere in your body.
- There have also been reports of cross transmission of hepatitis B, hepatitis C or HIV between patients in a dialysis centre, though the rates are low. You should be vaccinated against hepatitis B before starting hemodialysis treatment.
- The AVF may clot with prolonged use or could get infected.
- Because heparin is being used during the treatment, your blood may not be able to form clots, resulting in an increased risk of bleeding. If you are going for any surgical or dental procedure, you should inform your kidney specialist ahead of time, so that he or she can adjust your heparin prescription during the dialysis.
Peritoneal Dialysis (Water-Based form of dialysis treatment)
What is Peritoneal Dialysis?
- Peritoneal dialysis or PD is a water-based form of dialysis treatment, where a cleansing fluid called PD solution is instilled through a tube into the abdominal cavity and allowed to dwell for a certain number of hours.
- PD uses the natural membrane surrounding the abdominal cavity and organs to perform the dialysis.
- Toxins and excess water are extracted by the PD solution into the abdominal cavity, and these are then drained out together with the PD solution at the end of the dwell. We call each dwell a PD exchange.
What are the preparations required?
- To instill and drain PD solutions, a silicon tube called a PD catheter needs to be inserted into the abdominal cavity. This is a simple surgery which is usually performed in a day surgery setting.
- The diameter of the PD catheter is usually about 5 millimeters and will protrude out of an opening (called the exit site) from your abdomen around the umbilicus region.
- The catheter can be coiled and be hidden underneath your clothes.
- Ideally, the surgical site should be completely healed before PD can be performed, and a waiting time of about 2 weeks after the PD catheter insertion is preferred.
- PD is performed by the patient or any lay person looking after the patient at home. As such, the person performing the PD exchanges will need to undergo a period of training of about 3-5 days.
- Your kidney specialist will arrange for the company to deliver the supplies of PD solutions to your home, usually on a monthly basis.
- Some modifications to your home may be necessary to create storage space for these solutions, or to improve lighting and allow appropriate handwashing to be performed during each PD exchange. Your kidney specialist will review these requirements with you before starting PD treatment.

How is Peritoneal Dialysis performed?
- PD can be performed either manually or through a machine, called automated PD. Manual PD is usually performed in the daytime, while automated PD happens at night when the patient is sleeping.
- PD is a gentler form of dialysis and is usually performed daily. However, the flexibility of the PD therapy allows your kidney specialist to adjust the number of exchanges over the week, such that fewer exchanges could occur on weekends or that PD exchanges could be omitted on a certain day depending on your medical condition.
-
Manual PD:
- Each exchange takes about half an hour, and patient can perform about 3-5 exchanges a day, depending on their medical condition.
- During an exchange, the PD catheter is connected to the tubing from the PD solution bag. The PD solution in the abdominal cavity from the previous exchange is drained into an empty bag connected to the tubing. This usually takes about 20 minutes.
- The fresh PD solution will then be allowed to drain into the abdominal cavity. The volume of the PD solution can be adjusted by your kidney specialist but it is usually about 2 litres. This process usually takes about 10 minutes.
- Once the new PD solution is completely instilled into the abdominal cavity, the PD catheter is disconnected and capped up.
- The PD solution will be allowed to dwell in the abdominal cavity for 4-6 hours, to allow the dialysis to happen. During this time, the patient can go about his or her activities without the restriction of being hooked up to a machine.
- Longer dwell times may be allowed depending on your condition and the type of PD solution used. You should discuss this with your kidney specialist, so that your PD treatment can be personalized according to your needs and lifestyle.
-
Automated PD:
- This is performed at night when the patient is about to sleep, using a machine to perform the exchanges throughout the night.
- Preparation is made to connect the PD solutions needed for the entire treatment to the machine.
- The PD catheter from the machine is then connected to a tubing from the machine, and the necessary information is keyed into machine.
- At the press of a button, the PD exchanges will proceed throughout the night. Each machine treatment is usually about 8 to 10 hours.
- At the end of the treatment, the machine may drain the abdominal cavity completely dry or may instill a certain volume of fluid into the abdominal cavity, depending on the prescription decided by your kidney specialist.
- The PD catheter is then disconnected and capped up, and the patient can go about the day’s activities without restriction.
- If there is solution in the abdominal cavity throughout the day, this is first drained out by the machine during the subsequent night’s PD treatment.
What are the risks of Peritoneal Dialysis?
- Bacteria could enter through the tubing into the abdominal cavity and cause infection, called peritonitis. However, there had been reports of patients staying infection-free for years if hand hygiene is observed and the PD exchanges are performed correctly.
- The exit site where the PD catheter protrudes from the abdomen may get infected. Patients will be taught how to clean the area regularly to minimize infection risks.
- The catheter in the abdominal cavity may migrate or become blocked by the fat tissues in the abdomen, causing the flow of the PD solution to be disrupted. This is often caused by constipation, so it is important for patients to ensure regular bowel movement and sometimes laxatives may be necessary.
- The PD solution usually contains sugar and this may cause the blood sugar levels to be high in patients who have diabetes. Your kidney specialist may adjust your diabetes medications when you start the PD treatment so that your blood sugar level can remain controlled.
- Because your abdomen will contain about 2 litres of fluid during the PD exchange, the pressure in your abdomen will increase and you may experience some breathlessness or bloatedness. Sometimes, the abdominal pressure may be high enough to cause hernia or genital swelling. Your kidney specialist will be able to adjust the volume of PD solution to minimize these occurrences.
Kidney Transplantation
Kidney transplantation remains the best treatment for people with advanced kidney failure. However, not all patients are suitable for a transplant. Do discuss with your kidney specialist on the option of kidney transplantation, and how best to proceed with a kidney transplantation should you be considered suitable for this treatment.

What is Kidney Transplantation?
- Kidney transplantation involves the removal of a health kidney from a donor and surgically implant it into a patient with kidney failure.
- Because the new kidney is an organ foreign to the kidney transplant recipient, the patient will need to take medication to suppress the immune system from rejecting the transplanted kidney.
Suitability for a kidney transplant
- Kidney transplantation is the best treatment option for patients with advanced kidney failure, and anyone who is suitable should receive a kidney transplantation when possible.
- However, not all patients are suitable for a kidney transplant. Your kidney specialist will assess the safety of you undergoing general anaesthesia and the surgical procedure of a transplant, depending on your overall health and medical conditions.
- In addition, as medications are required to suppress your immune system, your kidney specialist will also need to assess you for risks of infections and cancer, that may flare up when your immune system becomes weakened.

Assessing the kidney donor
- The best outcomes for a kidney transplant occur with a living donor, especially if the donor is related to the patient.
- Likewise, the kidney specialist will need to ensure that the donor is healthy and it is safe for him or her to undergo general anaesthesia and to have the surgery to remove one kidney.
- In addition, the kidney specialist will also have to determine that the risk of the donor developing kidney failure after the transplant or in the future, is low enough for him or her to donate a kidney.
- Your donor will also be screened for infections and unknown cancers that could potentially be transmitted to the recipient during the transplantation.
Risks associated with a kidney transplant
- There are risks associated with general anaesthesia the actual surgical procedure. Bleeding, infection and damage to surrounding structures are risks associated with any surgical procedure. Your kidney specialist will arrange for you to have an in-depth discussion with the anaesthetist and transplant surgeon before the actual procedure.
- As drugs are required to suppress your immune system, you will be at a higher risk for infections and cancers. Your kidney specialist will start you on medications that may protect you from certain infections, and arrange for you to undergo cancer screening regularly.
- There is always a risk that the new kidney may not work despite all measures to maximize the outcome before, during and after the transplant.
- Despite the medications to suppress your immune system, your body may continue to reject the transplanted kidney. When a rejection occurs, your kidney specialist will attempt to salvage the kidney with medications or specialized treatment. However, sometimes a rejection is severe enough that the kidney will stop functioning and you will need to go back on dialysis.

Dr Adrian Liew
留成竹医生
MBBS, MRCP(UK), FAMS, FRCP(Edin),
FASN, MClinEpid
Senior Consultant Nephrologist and Director
Dr Adrian Liew is a Senior Consultant and kidney specialist with a vast experience in the management of patients with general medical and kidney conditions. He holds several leadership positions in the international kidney medicine community and has been invited to develop clinical practice guidelines for the care of patients with diabetic kidney disease, glomerulonephritis and who are on dialysis.
Read More